
Insulin is absorbed from the depot under the skin and into the bloodstream. From there, it continues on to the cells who put it to work.

Insulin hexamers must break down into monomers and dimers before they can enter the bloodstream via the capillaries.
After you inject insulin, it goes into the bloodstream to work. [1] If the insulin is R/neutral or one of the non-mixed analogs, it will be absorbed quickly. Fast-acting insulins are designed to be absorbed even faster, while insulin suspensions are made to "hinder" the rapid absorption of the insulin, to make them work for a longer time period.
The importance of how insulin is absorbed after it is injected under the skin is illustrated in this 2002 ADA Diabetes Care study, where short-acting R/Neutral and long-acting Lantus were compared when given intravenously, as opposed to subcutaneous use. Researchers found nothing slow-acting about Lantus when it was given intravenously, and they concluded that it is the absorption process from beneath the skin which produces the quite different effects these two have. [2]
Absorption varies from patient to patient; this is why some patients get more or less duration from an insulin than another patient using the same thing. [3]. It also can vary for the individual patient from day to day. [1] Absorption is one of the factors in insulin variability [4][5] The variability factor in persons with diabetes can be anywhere from 15-50% from one day to the next. [6]
Neutral[]
Insulin hexamers must break down into dimers and monomers to be absorbed. [7]
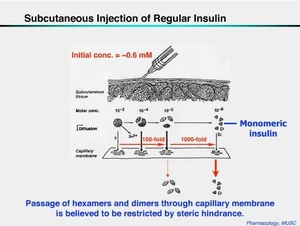
What happens after insulin is injected subcutaneously. It must break down from its hexamer form into dimers and monomers before it can enter the bloodstream via the capillaries to go to work on reducing blood glucose.
Neutral or R insulin is basically zinc insulin crystals dissolved in clear fluid with nothing added to alter its action or speed. [8]. This is true regardless of the insulin's species of origin; it has a normal absorption profile. Insulin molecules clump together naturally into "hexamers" (groups of six), which then drift apart when sufficiently diluted. The clumped form of hexamers, cannot be used directly, so there's a bit of time delay using R insulin while they are broken down into dimers and monomers.
It might be easier to visualize this by thinking of a whole pie, slicing it into 6 pieces and putting one slice each on separate plates. The pie can't be eaten until it has been cut and served on plates.
While the body stores insulin in hexamer form, [9] a normally working pancreas secretes it in monomer form, so there's no formation of hexamers by self-association and nothing to break down; the monomer insulin is ready to work. [10]
Faster-acting[]
It is possible to "speed" the absorption of insulin; one way is to alter the amino acid sequence(s) of them, producing analog insulins like Humalog, Novolog, NovoRapid and Apidra. Some of these (Humalog, Novolog) work by substituting or exchanging one or two amino acids at or near positions B-#28 & B-#29 so that insulin molecules will tend to remain separate instead of allowing them to clump together naturally into hexamers. [11] Apidra's substitutions are a bit different-at B-#3 and B-#29. [12] Using these types of alterations to force the insulin molecules to dissociate (remain apart, in the form of dimers and monomers, rather than their natural tendency to stay together), means they will be absorbed by the body faster.
Another way of forcing the insulin hexamers to stay apart and speed their absorption is with a less than U100 strength of insulin. Diluting insulin into U40 strength forces them into dissociating (staying apart from each other, and becoming dimers and monomers), which means they are absorbed [13][14] better and more rapidly. [15][16][17]
This study compares the absorption rate of U100 and U40 insulins. [18]. The findings show U100 insulin to be significantly slower acting than U40 because it has a slower absorption rate. (Note the same study is available through a URL from Diabetes Care--a publication of the American Diabetes Association.) [19] From 30-40 minutes after injection, U40 insulin produces a 20% higher insulin level in the body than the identical amount of U100 insulin injected at the same time. U40 insulin often has a faster onset then does U100 insulin. [7]
U40 insulin [20] was also the subject of another 1998 study. This one compared it to both U100 insulin and the rapid-acting analog insulin Lispro (The only one marketed at the time.). Insulin lispro, known as Humalog, was found to be only slightly more rapidly absorbed than U40 non-analog insulin. The rapid-acting analog insulins such as Humalog, Novolog, NovoRapid and Apidra have amino acid sequences which are altered to prevent the insulin hexamers from remaining together in self-association. Diluting insulin from U100 strength also prevents this self-association. [15]
The fact that U40 insulin has a similar pharmacokinetic profile to rapid-acting analog insulin, has not been lost on the German Institute for Health Care Quality (government department). They proposed a cost-cutting move which would limit prescription coverage of the rapid-acting analogs in Germany. [21]
Slower-acting[]
Other insulins, whether suspended or not, contain minute crystals of varying sizes which are deposited under the skin with the injection. Those with larger crystals, such as Ultralente, are absorbed slower than those with microfine ones, such as Semilente. Lente-type insulins are a "blend" of 30% faster-acting semilente crystals and 70% slower-acting Ultralente ones; this produces an intermediate-acting insulin. Mixed insulins are combined with a protamine suspension to keep them from being absorbed rapidly. [22][17]
Though it is not a suspended insulin, Lantus delays its absorption by not forming crystals until AFTER it has been injected and also via alterations made to the basic human insulin molecule. [23] Lantus's suspension is a special acidic preparation (pH 4.0) that reacts with the injection site forming micro-precipitates around the insulin crystals, which keeps them trapped for a while. Once the crystals make it to the bloodstream, they're absorbed as fast as any other insulin. Don't rub the injection site after injection or you can speed up absorption of Lantus and all other insulins. [24][25]
Levemir has a genetically-engineered sticky "acyl side chain" that clings for a while to albumin (protein) molecules found in the bloodstream (and under the skin) that makes the Levemir molecule too big to enter/exit the bloodstream and therefore slows down its absorption, not only at the site but also in the bloodstream and at the target tissues.

Humulin R U 500 strength. Note that the vial is 20 ml--twice the size of the standard 10 ml ones and the striping on the carton to alert users to the fact that this insulin is 5 times the strength of standard U 100 insulins. [26]
It is also possible to delay the absorption of an insulin by increasing the strength of its concentration. [17] U500 insulin, which is five times more concentrated than U100 [27], has been available through both Lilly and Novo Nordisk (Note: Their similar product is U400 strength insulin [28]) by special order for many years. [29] The insulin's main use is for people with extreme Insulin resistance, and is commercially available only in R/Neutral type.
Though it is R/Neutral-type insulin, U400 & U500 insulins [30] have a pharmacokinetic profile more like NPH insulin than U100 R/Neutral. [4][26]
Since there are no additives such as suspensions to alter R/Neutral insulin's action, the strength of the insulin formula hinders its breakdown into dimers and monomers, thus making it much slower-absorbed than U100 and lesser strength insulins. [31][32][33]
In cases of severe insulin resistance, using a much higher concentration of insulin appears to "negate" the effects of immune-related insulin resistance.
The studies at the link below shows that there was no difference regarding antibodies when these patients were transferred from Iletin II NPH at U100 strength to a form of Iletin II R at U500 strength. However, the stronger insulin reduced their insulin needs from 33-75%. [34][35]
Whether the insulin is slowed by the size of its crystals, by its suspension, by the strength of its concentration, or by amino acid alterations designed to delay its absorption--all of these are different mechanisms with the same goal in mind--to keep the insulin in hexamer form (thus preventing its fast absorption) as long as possible.
Effect of origin[]
People absorb r-DNA/GE/GM insulin at a faster rate than an otherwise identical pork or beef insulin, [4][15][36][37] because it is an exact amino acid match to their own. [38][39] They absorb pork insulin a bit slower, because it is one amino acid away from theirs. [40][41] Slowest of all is beef insulin, as it is three amino acids away from a person's natural insulin. [42][43][44]
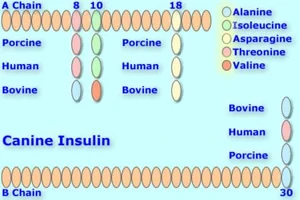
Canine insulin compared with Bovine, Human, & Porcine versions. Up to 2 amino acids differ with porcine and canine being identical. [45]
It would be exactly opposite for dogs because their natural insulin is a perfect match to pork insulin, and one amino acid away from r-DNA/GE/GM insulin. Dogs would absorb pork insulin faster than an otherwise identical r-DNA/GE/GM human insulin.[46] They would absorb beef insulin slower than either pork or r-DNA/GE/GM human insulin, as it is two amino acids away from a perfect match to their own. [17]
Origin, species, or source is very important as it directly affects the absorption, peak and duration of an insulin. [47]
Beef insulin, which is quite slow for human beings, [48] owing to the three amino acid difference between beef insulin and a human's own, would act more rapidly in cats, since it is the closest match we have to native feline insulin until r-DNA/GE/GM feline insulin comes along. Cats would absorb pork insulin slower than an otherwise identical beef insulin because of the 3 amino acid differences between them; they would absorb r-DNA/GE/GM human insulin slowest of all, because there are 4 amino acid differences in feline and human insulin. [49][50]
Effect of injection site[]
Taking absorption outside the lab, many other factors come into play. [17] A study done at the University of Minnesota showed that there is an 29-39% variation on the amount of insulin going into the bloodstream from one day to another. [51]
Absorption is faster when insulin is injected into limbs which are in motion [4][52] than in injection sites which are not--such as the back. Insulin also is absorbed faster via warmth--including the heat of summer. [53][52] When blood flow is increased to the site of the insulin injection, absorption also increases. [4]. Both warmth and movement of the injection site increase increase blood flow [14][4]
Some caregivers report differing absorption rates with the same insulin depending on the injection site, the shot technique, and the needle length on the syringe.
Absorption problems can occur possibly causing hypoglycemia [54] or hyperglycemia if the insulin injection sites are not varied. [55]
The area needn't be very far from where the last shot was given--the distance of the width of 2 fingers will do fine as a measure. [56]
When shots are given again & again into an area of skin, the tissue becomes thicker at that point; a fairly good analogy would be the calluses people get on hands and feet. The callus skin is thicker and harder; injection areas become similar to this too from repeated shots. This thicker, harder skin doesn't let the body absorb the injected insulin as well as thinner, non-hardened areas. [57]
Most of us dealing with pet diabetes vary the side we give the injections in--right side mornings and left side evenings, for example. This is another help in avoiding giving shots in the same areas. [58]
Many people give insulin shots in the scruff of the pet's neck, which is now considered to be a less than optimum choice. The neck area provides poor insulin absorption, due to it not having many capillaries, veins. etc. (vascularization).
Other sites suggested by Dr. Greco include the flank and armpit. [59]
Intervet recommends giving injections from just back of the shoulder blades to just in front of the hipbone on either side, from 1 to 2 inches from the middle of the back. [60]
Levemir has little feline or canine data, but the manufacturer claims [61] that in their testing on humans they found much lower day-to-day variability, even when shooting at different sites. They claim that this is because the Levemir "clinging" action [62] takes place throughout the body and in the blood, and so is not dependent on injection site conditions.
Depth of injection[]
Subcutaneous (under the skin) injections are absorbed the slowest. Intramuscularly (into the muscle) given ones are absorbed much faster, but should not be given other than on the advice of a medical professional. [52][17]
Insulin dose[]
The larger the dose of insulin, the longer it takes to be absorbed [63][17] and the more duration it will have. [52][64][65]
Effect of body condition[]
Dogs who are dehydrated may have reduced insulin absorption rates; vomiting and diarrhea can cause both dehydration and hypoglycemia from them. [66]
Dehydration can change the way subcutaneous insulin is absorbed. [67], causing either hyperglycemia or hypoglycemia [68]
Those with diabetes are at risk for dehydration as it is triggered by hyperglycemia. [69]
Other factors modulating insulin absorption [70] include regional blood flow which is affected by exercise,[71][72] rubbing or massage, [73] and temperature. [73]
Effect of needle length[]
Some caregivers report difference in insulin absorption with different length needles. BD Diabetes [74] explains that you should consult with your health care professional before using a short needle, and carefully monitor blood glucose when changing to a shorter needle.
People have found their blood glucose not well-controlled when switching to the shorter needles; this also has been the case with some dogs. Switching back to a longer needle solved the problem. You should consider experimenting with the different length needles as insulin absorption may vary. [75] ![]()
References[]
- ↑ 1.0 1.1 Disposition & Fate of Drugs. Merck Veterinary Manual.
- ↑ Intravenous Glargine (Lantus) & Regular (Neutral) Insulin Similar Effects on Endogenous Glucose Output & Peripheral Activation/Deactivation Kinetic Profiles. ADA-Diabetes Care (2002).
- ↑ Diabetes Forecast-page 2. American Diabetes Association (2006).
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 Questions About Insulin. Diabetes-World Mailing List. Cite error: Invalid
<ref>tag; name "Questions" defined multiple times with different content Cite error: Invalid<ref>tag; name "Questions" defined multiple times with different content Cite error: Invalid<ref>tag; name "Questions" defined multiple times with different content Cite error: Invalid<ref>tag; name "Questions" defined multiple times with different content Cite error: Invalid<ref>tag; name "Questions" defined multiple times with different content - ↑ Insulin Treatment-Individual Factors. Patients UpToDate.
- ↑ Schermerhorn, Thomas (2008). Strategies for monitoring diabetes mellitus in dogs. DVM 360.
- ↑ 7.0 7.1 Hanas, Ragnar (1999). Insulin Dependent Diabetes (page 5). Children With Diabetes. Cite error: Invalid
<ref>tag; name "Ragnar" defined multiple times with different content - ↑ Humulin R. US-FDA.
- ↑ Insulin. Wikipedia.
- ↑ Abrams-Ogg, Anthony (2007). Chemistry and Pharmacology of Therapeutic Insulin Preparations. ACVIM.
- ↑ Details Human Insulin Alterations for Humalog (Lispro), Novolog/NovoRapid (Aspart) & Lantus (Glargine}. Clinchem.org.
- ↑ Prescribing Information-Apidra. Sanofi-Aventis.
- ↑ Sindelka, G., Heinemann, L., Berger, M., Frenck, W., Chantleau, E. (1994). Effect of insulin concentration, subcutaneous fat thickness and skin temperature on subcutaneous insulin absorption in healthy subjects.. Diabetologica.
- ↑ 14.0 14.1 Hirsch, Irl (1999). Type 1 Diabetes Mellitus & Use of Flexible Insulin Regimens. American Family Physician. Cite error: Invalid
<ref>tag; name "Hirsch" defined multiple times with different content - ↑ 15.0 15.1 15.2 Hildebrandt, P. (1991). Subcutaneous Absorption of Insulin in Insulin-Dependent Diabetic Patients. Influence of Species, Physico-chemical Properties of Insulin and Physiological Factors. Danish Medical Bulletin.
- ↑ Pharmacokinetics vs Pharmacodynamics. Endotext.org.
- ↑ 17.0 17.1 17.2 17.3 17.4 17.5 17.6 Heinemann, Lutz (January 2008). Variability of Insulin Action:Does It Matter?-page 40 (4 of 9). Insulin Journal.
- ↑ Hildebrandt, P., Sesoft, L., Nielsen, SL (1983). The absorption of subcutaneously injected short-acting soluble insulin: influence of injection technique and concentration.. Diabetes Care.
- ↑ Copy of Reference in ADA's Diabetes Care Publication. American Diabetes Association.
- ↑ Polaschegg, E. (1998). Effect of physicochemical variables of regular insulin formulations on their absorption from the subcutaneous tissue. Diabetes research and clincal practice.
- ↑ Rapid-acting insulin analogues in diabetes mellitus type 1: Superiority not proven. IQWiG-German Institute for Quality and Efficiency in Health Care (6 June 2007).
- ↑ Pharmacokinetics vs Pharmacodynamics. Endotext.org.
- ↑ Owen, William E., Roberts, William L. (2004). Alterations of Human Insulin Producing Insulins Apart, Glargine & Lispro. Clinical Chemistry.
- ↑ Hanas, Ragnar. Insulin-Dependent Diabetes (pages 12 & 13). ChildrenWithDiabetes.
- ↑ Insulin Treatment-Factors Affecting Insulin Action. PatientsUpToDate.
- ↑ 26.0 26.1 Cochran, Elaine (2009). U-500 Insulin: When More With Less Yields Success. Diabetes Spectrum-American Diabetes Association. Cite error: Invalid
<ref>tag; name "Cochran" defined multiple times with different content - ↑ Humulin R 500. Revolution Health.
- ↑ Cochran, Elaine (2005). Use of U500 Insulin in Patients With Extreme Insulin Resistance. Diabetes Care-American Diabetes Association.
- ↑ Diabetes Forecast page 4. American Diabetes Association (2006).
- ↑ Insulins. Diabetes Monitor (September 2008).
- ↑ Jørgensen, KH, Hansen, AK, Buschard, K. (2000). Five Fold Increase of Insulin Concentration Delays the Absorption of Human Insulin Injections in Pigs. Diabetes Research & Clinical Practice.
- ↑ Lane, WS (2006). Use of U500 R Insulin by Continuous Insulin Infusion (Insulin Pump) in Patients With Type 2 Diabetes & Severe Insulin Resistance. Endocrine Practice.
- ↑ Humulin R-U500 Patient Leaflet. Eli Lilly.
- ↑ Nathan, DM, Axelrod, L, Flier, JS, Carr, DB (1981). U500 Insulin in the Treatment of Antibody-Mediated Insulin Resistance. Annals of Internal Medicine.
- ↑ Baumann, G, Drobny, EC (1984). Enhanced Efficacy of U500 Insulin in the Treatment of Insulin Resistance Caused by Target Tissue Insensitivity. Journal of the American Medical Association.
- ↑ Selam, JL, Turner, D, Woertz, L, Eichner, HL, Lauritano, A, Charles, MA (1989). Comparison of the Safety and Effectiveness of Human and Bovine Long-acting Insulins. Diabetes Research.
- ↑ Faster Onset & Shorter Duration of GE Insulin in Humans. Diabetes Health.
- ↑ Sailer, D, Ludwig, T, Kolb, S. (1982). Comparing Activity Profiles of GE R(Neutral)/NPH(Isophane) With Different Fractions to Fixed-Fraction (70/30--30/70) Pork Mixed Insulin (Pork Mixtard 30).
- ↑ Owens, DR, Vora, JP, Heding, LG, Luzio, S, Ryder, RE, Atiea, J, Hayes, TM. (1986). Human, Porcine and Bovine Ultralente Insulin: Subcutaneous Administration in Normal Man. Diabetic Medicine.
- ↑ Richard, JL, Rodier, M, Cavalié, G, Mirouze, J, Monnier, L. (1984). Human & Porcine NPH (Isophane Insulins Unequally Effective in Diabetic Patients. Acta Diabetologica Latina.
- ↑ Renner, R, Vocke, K, Hepp, KD. (1986). Comparison of Effects of Protamine-Bound NPH (Isophane) Porcine Insulin & NPH (Isophane) Human Insulin in T1 & T2 Diabetes. Deutsche Medizinische Wochenschrift (Translated into English).
- ↑ Marre, M, Tabbi-Anneni, A, Tabbi-Anneni, H, Assan, R. (1982). Comparison of NPH (Isophane) Human Insulin & NPH (Isophane) Bovine Insulin in Humans. Diabetes Care-American Diabetes Association.
- ↑ Hirsch, Irl, Farkas-Hirsch, R. (1993). Type I Diabetes and Insulin Therapy. Nursing Clinics of North America.
- ↑ Marre, M, Tabbi-Anneni, A, Tabbi-Anneni, H, Assan, R. (1982). Comparative Study of r-DNA NPH Insulin and Bovine NPH Insulin in Humans. Diabetes Care.
- ↑ Caninsulin Product Information. Intervet.
- ↑ Greco, Deborah (2010). Treating Diabetes Mellitus in Dogs and Cats. Western Veterinary Conference.
- ↑ Diabetes Forecast-page 3 (2006).
- ↑ Insulin Therapy-Overview. RxEd.
- ↑ Bovine PZI Insulin. BCP Veterinary Pharmacy.
- ↑ Broussard, JD, Peterson, ME. (1995). Comparison of 2 Ultralente Insulin Preparations With Protamine Zinc Insulin in Normal Cats. American Journal of Veterinary Research.
- ↑ Bernstein, Richard. Day To Day Variability Of Insulin. Diabetes In Control.
- ↑ 52.0 52.1 52.2 52.3 Schaer, Michael (2008). Diabetic Phenomena. WSAVA. Cite error: Invalid
<ref>tag; name "Schaer" defined multiple times with different content Cite error: Invalid<ref>tag; name "Schaer" defined multiple times with different content Cite error: Invalid<ref>tag; name "Schaer" defined multiple times with different content - ↑ Diabetes Mellitus Treatment. PetHealth101.
- ↑ Insulin-Section 6.1-Kinetics. InChem.
- ↑ Cook, Audrey (1 April 2010). Identifying the reasons behind difficult-to-control diabetes in dogs. DVM 360.
- ↑ Tips for Injecting Insulin. Joslyn Diabetes Center.
- ↑ Injection Site Selection. BD Diabetes.
- ↑ Greco, Debra. FAQ's About Diabetic Dogs. BD Diabetes.
- ↑ Better Medicine E-Newsletter. Intervet USA (June 2006).
- ↑ Vetsulin-Preparing Insulin & Giving Injection-Page 2
- ↑ Levemir--Less Variability. Novo Nordisk.
- ↑ Levemir "Clinging" Action Movie. Novo Nordisk.
- ↑ Bernstein, Richard. The Law of Small Numbers Part 2. Diabetes In Control.
- ↑ King, Scott (2007). Why Smaller Shots of Insulin Get Absorbed Faster, Peak Sooner, and Are Out of Your System Quicker. Diabetes Health.
- ↑ Fischer, U, Freyse, EJ, Jutzi, E, Besch, W, Raschke, M, Höfer, S, Albrecht, G. (1983). Absorption rates of subcutaneously injected insulin in the dog as calculated from the plasma insulin levels. Diabetologia.
- ↑ Diabetes and Travel-page 4. DiabetesNow-UK.
- ↑ Pediatric Endocrine Emergency Answer Sheet. American College of Emergency Physicians.
- ↑ Diabetes and Travel-page 4. DiabetesNow-UK.
- ↑ Hyperglycemia. FAQS.org.
- ↑ Hirsch, Irl. Insulin in the Hospital Setting-page 8. U of Washington Medical Center.
- ↑ Insulin Treatment-Factors Affecting Insulin Action. PatientsUpToDate.
- ↑ Variables affecting chemistry results. Cornell University.
- ↑ 73.0 73.1 Hanas, Ragnar. Insulin Dependent Diabetes in Children, Adolescents and Adults-page 11-Factors Influencing the Insulin Effect. ChildrenWithDiabetes.
- ↑ Using Short Needles. BD Diabetes.
- ↑ ADA Position Statement. American Diabetes Association (2004).
See also duration, peak, onset, carryover and Insulin.
More Information[]
- Absorption Kinetics of Regular (Neutral) & Isophane (NPH) Insulin in the Normal Dog Goeders LA, Esposito LA, Peterson ME., Domestic Animal Endocrinology, 1987
- Mechanism for Novolog (pdf) Novo Nordisk
- Mechanism for Humalog (pdf) Eli Lilly
- A chart of the variations in amino acid sequence on the A and B chains of different species Pet Diabetes
- Drug Absorption from Parenteral (injected) Delivery Sites Merck Veterinary Manual
- Variability of Insulin Action-Does it Matter Heinemann, Lutz, Insulin Journal 2008
- Absorption of Insulin Richards, Mike, Vet Info 4 Dogs